For more than two decades, researchers have tried to regenerate injured optic nerves using different growth factors or agents that overcome natural growth inhibition. They’ve had partial success, sometimes even restoring rudimentary elements of vision in mouse models.
But at best, these methods get only about 1 percent of the injured nerve fibers to regenerate and reconnect the retina to the brain. That’s because most of the damaged cells, known as retinal ganglion cells (RGCs), eventually die, says Larry Benowitz, Harvard Medical School professor of neurosurgery at Boston Children’s Hospital.
Benowitz and colleagues have found a surprising new approach that gets RGCs to live longer and regenerate robustly: using chelating agents to bind zinc that’s released as a result of the injury.
These studies were done in mice. If the findings hold up in human studies, they could spell hope for people with optic nerve injury due to trauma, glaucoma or other causes, and possibly even spinal cord injury, the researchers said.
The results were published Jan. 2 in PNAS.
A spike in zinc
Until now, what actually kills RGCs after optic nerve injury hadn’t been known.
“At least 200 studies, including some done here, have tried to understand what makes these cells die,” said Benowitz, who is also a member of the F.M. Kirby Neurobiology Center at Boston Children’s. “And even if the cells survive, they usually cannot regrow their connections.”
Benowitz’s colleague, Paul Rosenberg, HMS associate professor of neurology at Boston Children’s, suggested looking at zinc in the retina. He had already been studying the role of zinc in the death of nervous system cells and knew that in many neurons zinc is packaged together with the neurotransmitters used to communicate with other cells.
The Rosenberg and Benowitz labs began collaborating in 2010, led by Yiqing Li, HMS instructor in neurosurgery at Boston Children’s.
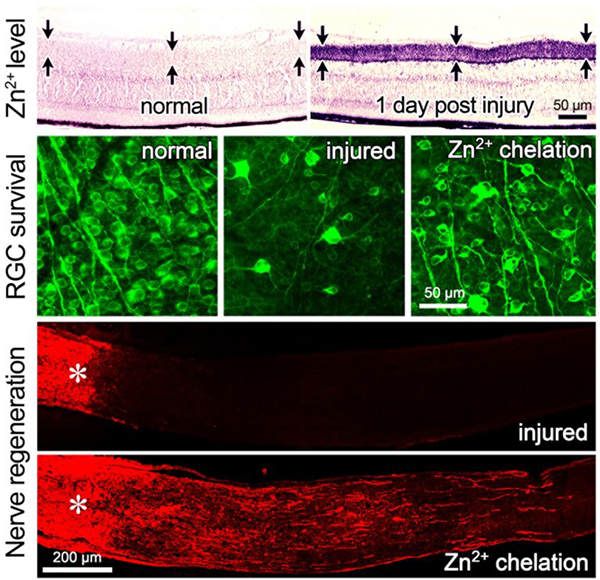
Zinc release is normally tightly controlled, because high levels are toxic to cells. But within an hour after injury to the optic nerve, the researchers watched zinc spike—not in the damaged RGCs themselves but in cells that talk to them, interneurons known as amacrine cells.
Two or three days later, the zinc transferred to the RGCs. Only then did the cells begin to die.
A window of treatment opportunity?
This time lag offers a potential window for intervention.
The researchers observed robust cell survival and axon regeneration even if treatment was delayed for as much as five days. Regeneration was further enhanced when the team combined chelators with deletion of the pten gene to decrease natural growth inhibition.
Zinc chelators already exist and could potentially be given systemically or through direct injection into the eye after an optic nerve injury, the researchers said.
The team hopes to get further funding to develop a slow-release formulation that would chelate zinc over a period of time. This could allow patients to receive just a single injection.
“When we used zinc chelators, we enabled about 40 percent of the injured cells to survive for months and possibly indefinitely,” said Benowitz. “Growth factors and survival factors only have a transient effect; they don’t really stop the cell death process. If you hit the right dosage and deliver zinc chelators continuously, you might have half of the retinal ganglion cells surviving.”
Zinc: The new calcium?
Benowitz, Rosenberg and Li are also interested in exploring how zinc causes cell death and blocks regeneration.
“We think more ideas for new therapeutic approaches could come out of these investigations,” said Rosenberg.
While this is the first study to demonstrate the role of zinc in optic nerve injury, zinc has also been shown to play a role in stroke injury and has been implicated in Alzheimer’s disease and amyotrophic lateral sclerosis.
“Very little is known about the role of zinc in the healthy nervous system or its role in brain injury, although through the work of many groups around the world we are beginning to appreciate its significance,” said Rosenberg. “Everyone has thought of calcium as the master regulator in health and disease. We think zinc will come to share that role in the 21st century.”
Adapted from a post on Vector, the Boston Children’s science and clinical innovation blog.




