Investigators from Harvard Medical School, Massachusetts General Hospital, and the Ragon Institute of MGH, MIT and Harvard have added another piece to the puzzle of how a small group of individuals known as elite controllers are able to control HIV infection without drug treatment.
In their paper published in the journal PLOS Pathogens, the research team reports finding that dendritic cells of elite controllers are better able to detect the presence of HIV—paradoxically through a greater susceptibility to HIV infection—which enables them to stimulate the generation of T cells specifically targeting the virus.
“It’s been recognized for a while that these individuals have stronger T-cell immune responses against HIV than other patients, but the reason for that has been unknown,” said Xu Yu, HMS associate professor of medicine at Mass General and corresponding author of the paper. “We have shown that dendritic cells, which play a critical role in generating virus-specific T cells, have an improved ability to recognize HIV and build effective immune responses in elite controllers.”
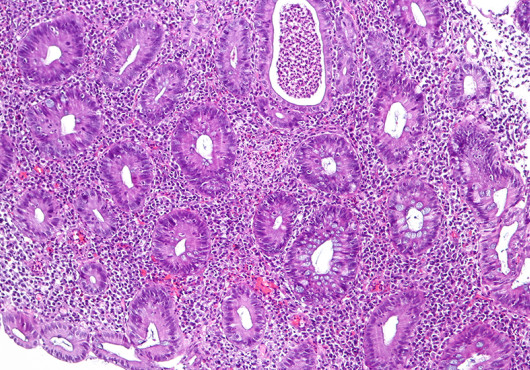
Part of the innate immune system that is the body’s first line defense against infection, dendritic cells sense the presence of pathogens in the blood or other tissues, ingest infecting organisms and then display fragments of the invaders on their surface, which alerts and activates both killer and helper T cells (CD4 and CD8 cells), essentially teaching them to target the specific pathogen.
Because of this critical role of dendritic cells, the investigators explored the hypothesis that dendritic cells of elite controllers were better able to sense HIV and, as a result, better able to generate virus-specific T-cell responses.
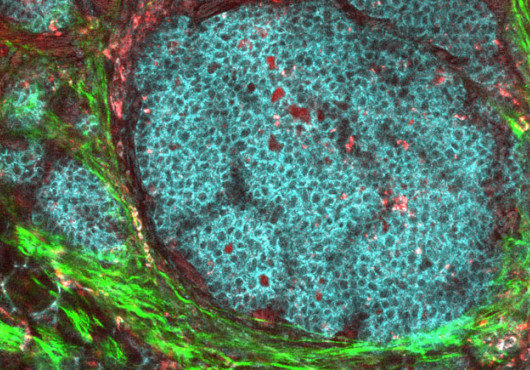
When HIV infects a cell, it first injects its genetic material—RNA in this case—into the cell along with the reverse transcriptase enzyme that transcribes the single-strand RNA molecule into a double-stranded DNA molecule. After HIV DNA enters the nucleus of an infected cell, it becomes integrated into the cellular DNA, turning it into an HIV factory that generates more virus particles.
In experiments using dendritic cells from elite controllers, from patients with progressing HIV infection, and cells from uninfected individuals, the investigators found a surprising difference. In most people, HIV infection of dendritic cells appears to be blocked at an early stage, resulting in a lack of HIV DNA and limited viral replication within those cells. While this may seem beneficial, it actually works more to the benefit of the virus than the infected individual by allowing HIV to escape recognition by dendritic cells.
The dendritic cells of elite controllers, however, were found to contain higher levels of HIV DNA, probably because of limited expression of a protein called SAMDH1 that usually blocks reverse transcription in several types of immune cells. The dendritic cells of elite controllers also appear to produce higher levels of a DNA-sensing protein called cGAS that recognizes the presence of HIV and induces rapid expression of type 1 interferons. This contributes to the generation of the more powerful T-cell responses against HIV that are typically observed in elite controllers.
“We are now focusing on fully understanding all the components required to trigger appropriate activation of dendritic cells in HIV infection, which may help to induce an elite-controller-like, drug-free remission of HIV in a broader patient population,” Yu explained.
Support for the study includes National Institutes of Health grants AI078799, AI089339, L121890, AI098484, HL126554, AI116228, AI087452, AI098487 and AI106468.
Adapted from a Mass General news release.