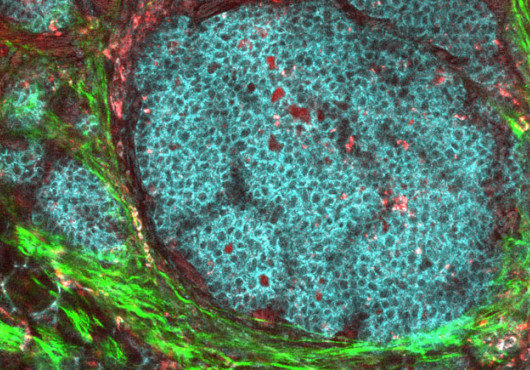
The onset of Alzheimer’s disease (AD), an irreversible neural disorder, has been linked to the production of beta-amyloid proteins in the brain. These short, unfolded proteins associate with one another to form aggregates, which eventually amass into insoluble plaques that wreak havoc on neurons (see figure).

For years, researchers have believed beta-amyloid to be a protein byproduct that serves no physiological function. Because of this, therapies aimed at reducing the concentration of these proteins in the brain have been developed. Recently, however, Robert Moir, an HMS assistant professor of neurology, and Rudolph Tanzi, the Joseph P. and Rose F. Kennedy professor of child neurology and mental retardation, both at Massachusetts General Hospital, and colleagues have published a groundbreaking study in which they provide the first evidence that beta-amyloid production may be the consequence of a genuine immune response. The discovery suggests that AD occurs when this process is improperly regulated.
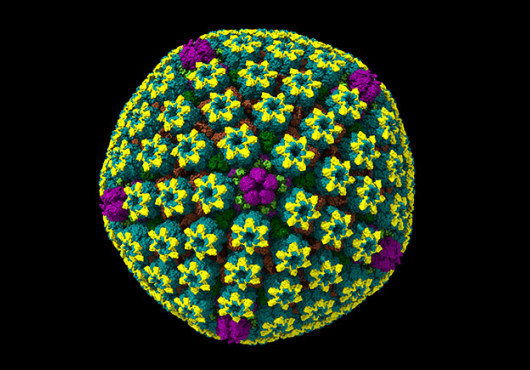
In their report, published online March 3 in PLoS One, the researchers show that the beta-amyloid protein linked to Alzheimer’s has antimicrobial activity similar to and, in some cases, greater than LL-37, a known human immune defense peptide. Beta-amyloid also kills eight strains of bacteria that cause human infection. In fact, brain tissue samples taken from AD patients were able to kill bacteria more readily than non-AD tissues, and this antimicrobial activity was diminished when the beta-amyloid protein was rendered inactive through antibody binding. The researchers propose that humans may produce these molecules as part of an immune response to clear a bacterial infection.
These findings have implications for the treatment of Alzheimer’s disease because current therapeutic strategies aimed at halting the production of these proteins may impair patients’ immune responses. The study suggests that alternative therapeutic strategies to dial down the production of beta-amyloid, without eliminating it, should be explored.
For more information, students may contact tanzi@helix.mgh.harvard.edu.
Conflict Disclosure: The authors declare no conflicts of interest.
Funding Sources: Cure Alzheimer’s Fund; the authors are solely responsible for the content of this work.