Getting enough sleep is key to good health, and studies have shown that insufficient sleep increases the risk of serious problems, including cardiovascular disease. Now, Harvard Medical School researchers based at Massachusetts General Hospital have discovered one way that sleep protects against atherosclerosis, the buildup of arterial plaques.
In their paper receiving advance online publication in Nature, the researchers describe the mechanism by which insufficient sleep increases production of inflammatory white blood cells known to be major contributors to atherosclerosis.
“We have discovered that sleep helps to regulate the production in the bone marrow of inflammatory cells and the health of blood vessels and that, conversely, sleep disruption breaks down control of inflammatory cell production, leading to more inflammation and more heart disease,” said Filip Swirski, HMS associate professor of radiology at Mass General and senior author of the Nature paper.
“We also have identified how a hormone in the brain known to control wakefulness controls processes in the bone marrow and protects against cardiovascular disease,” he said.
To investigate how insufficient sleep increases atherosclerosis, Swirski’s team subjected mice genetically programmed to develop atherosclerosis to repeated interruptions of their sleep, similar to the experience of someone constantly waking up because of noise or discomfort.
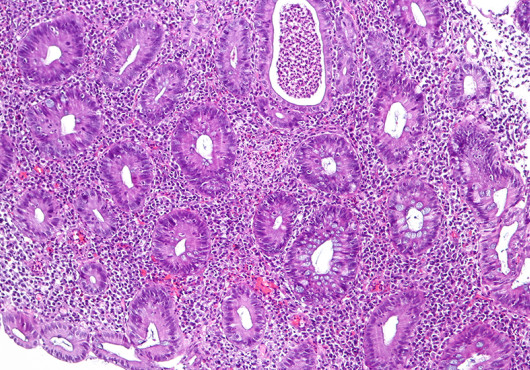
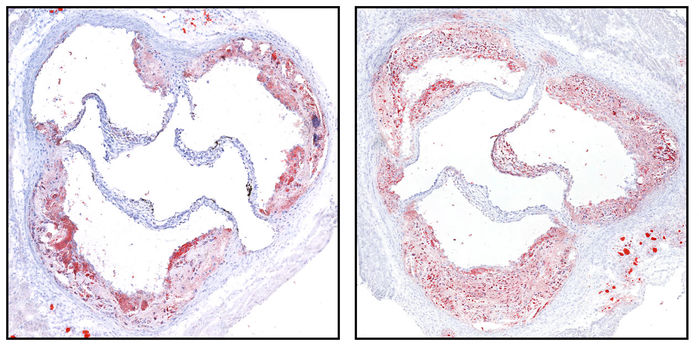
While there were no changes in weight, cholesterol levels or glucose tolerance in the sleep-deprived mice, compared to animals from the same strain allowed to sleep normally, those subjected to sleep fragmentation developed larger arterial plaques and had higher levels of monocytes and neutrophils—inflammatory cells that contribute to atherosclerosis—in their blood vessels.
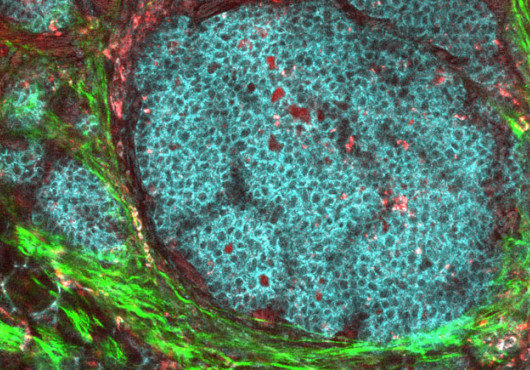
Further experiments revealed that the sleep-deprived mice had a nearly twofold increase in the production of stem cells in the bone marrow that give rise to white blood cells. Hypocretin, a hormone produced in the hypothalamus and known to have a role in the regulation of sleep, was found to play an unexpected role in controlling white blood cell production.
While normally produced at high levels when animals—including humans—are awake, hypocretin levels were significantly reduced in the sleep-deprived mice.
The team found that hypocretin regulates production of white blood cells through interaction with neutrophil progenitors in the bone marrow. Neutrophils, they discovered, induce monocyte production through release of a factor called CSF-1, and experiments with mice lacking the gene for hypocretin revealed that the hormone controls CSF-1 expression, monocyte production and the development of arterial plaques. In sleep-deprived animals, the drop in hypocretin led to increased CSF-1 production by neutrophils, elevated monocyte production and accelerated atherosclerosis.
“This is a direct demonstration that hypocretin is also an important inflammatory mediator,” said Swirski, who is a member of the Mass General Center for Systems Biology. “We now need to study this pathway in humans, explore additional mechanisms by which proper sleep maintains vascular health and further explore this newly identified neuro-immune axis.”
Additional authors include Cameron McAlpine, Máté Kiss, Christoph Binder, Peter Libby, Anne Vassalli, Mehdi Tafti, Thomas Scammell and Matthias Nahrendorf.
Support for the study includes National Institutes of Health grants R35 HL135752, R01 HL128264 and P01 HL131478 and the American Heart Association Established Investigator Award. Swirski is the Patricia and Scott Eston Mass General Research Scholar.
Adapted from a Mass General news release.