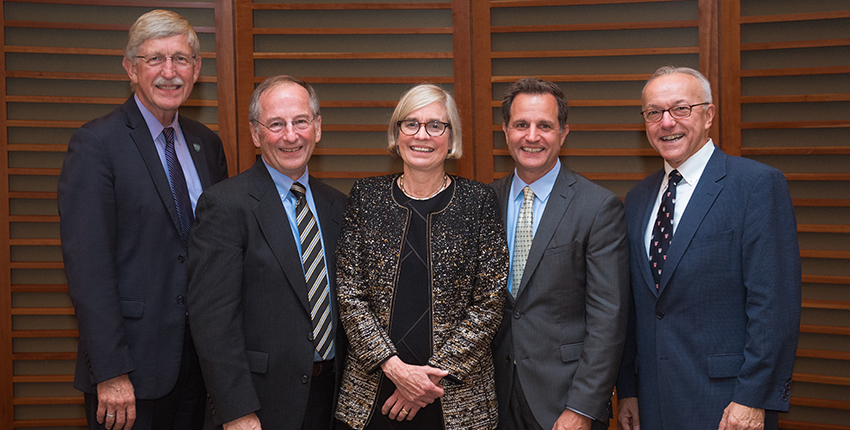
From left: Award recipients Francis Collins, Michael Welsh, Bonnie Ramsey, Paul Negulescu with Dean George Q. Daley. Image: Gretchen Ertl
You know it’s not your average science symposium when the director of the NIH, guitar in hand, leads the audience in song. On Thursday, Oct. 4, at Harvard Medical School, Francis Collins gave science a decidedly poetic twist by performing a ballad he composed to celebrate advances in the understanding and treatment of cystic fibrosis (CF).

Collins’ performance was part of the Warren Alpert Symposium—an annual event that recognizes scientistswhose work has improved the understanding, prevention and treatment or cure of human disease.
Collins was one of five recipients of the2018 Warren Alpert Foundation Prize, which honored transformative discoveries in the fields of genetics, physiology, pulmonology and pharmacology that led to life-altering precision-targeted treatments for CF, a rare and devastating multiorgan disease that affects nearly 75,000 people in the United States, Canada, Europe and Australia.
Other recipients included Paul Negulescu, senior vice president for research, Vertex Pharmaceuticals; Bonnie Ramsey, vice chair and endowed professor of pediatrics, University of Washington School of Medicine and director, Center for Clinical and Translational Research, Seattle Children’s Research Institute; Lap-Chee Tsui, founding president, The Academy of Sciences of Hong Kong; university professor emeritus, University of Toronto; and Michael Welsh, professor of internal medicine—pulmonary, critical care and occupational medicine, University of Iowa. Tsui was unable to attend the ceremony.
The arc of precision medicine
The hallmark of CF is a genetic mutation that impairs cells’ ability to transport chloride, leading to the accumulation of thick, sticky mucus in the lungs and other organs and causing a range of symptoms, most notably recurrent lung infections and progressive scarring and loss of lung function, as well as pancreatic, liver and other gastrointestinal problems.
CF was first recognized as a clinical syndrome in 1938. Life expectancy for infants born with CF at the time was 6 months of age.It has improved steadily over the past several decades, with the median age of survival in the United States and other developed countries now estimated to be in the 40s.
Yet, despite significant advances in diagnosis, treatment and care, until recently CF treatment remained more or less symptomatic. Thanks the discoveries made by the five award recipients, this is no longer the case. Collectively, their work has led to the development of precision-targeted medicines that correct the underlying protein defect that fuels disease development and its symptoms. In doing so, these therapies stave off organ damage and can boost survival.
The achievements of the five honorees “represent one of the most elegant and instructive protein-to-person trajectories in the history of biomedicine,” said George Q. Daley, dean of Harvard Medical School.
These achievements are the very essence of precision medicine, added symposium moderator Vamsi Mootha, professor of systems biology and medicine at HMS and Massachusetts General Hospital.Quoting from a State of the Union speech by former President Barack Obama, Mootha said that “in some patients with CF, precision medicine has reversed a disease once thought unstoppable.”
“To day is the most best day ever in my life. They found a Jean for cistik fibrosis.”
So reads the Aug. 25, 1989 entry from the diary of an 8-year-old girl with CF—written the same day that Collins and Tsui published their discovery describing the CF gene.
That entry, Collins said during his remarks at the symposium, was his favorite notation of these findings.
Collins and Tsui conducted the foundational work that culminated with the 1989 discovery of the CF gene, the elucidation of its molecular structure and function and its precise location. These findings provided an entry point to understanding the basic defect that fuels a complex disease affecting multiple organs and organ systems.
As a young physician-scientist, Collins said he had set out to understand the genetic underpinnings of inherited disorders he encountered in his genetics clinic but for which there was no molecular explanation.
Providing historical context, Collins described the 1980s as the medieval era of biomedical research—a time marked by a lack of sophisticated DNA analytic tools and only the vaguest notion of the size of the human genome.
At the time, Collins calculated his odds of pinpointing the CF gene. They were comparable to locating a 2,000-milligram needle in an eight-ton haystack, he said.
“We knew the human genome was somewhere in the neighborhood of 3 billion base pairs, and we knew we were looking for a single letter gone awry,” Collins said. “How the heck would you do that?”
For his gene-hunting odyssey, Collins sought a partner and found one in Tsui, a researcher in Toronto, who was also pursuing the elusive CF gene.
Collins recalled the close collaboration that ensued between the two teams—one marked by multiple drives between Ann Arbor and Toronto. The partnership culminated in the identification of the CF gene in May 1989—a feat the two researchers celebrated with a bottle of Canadian whiskey they’d agreed to open only in case of a success. They did so at 10 a.m. in the lab, much to the horror of the technician on site, Collins said.
The discovery of the CF gene has sparked daring scientific efforts across a broad range of disciplines, Collins said, including the Human Genome Project, the international research effort led by Collins himself, which culminated with the mapping of the entire human genome in 2003.
“I am not sure we’d have had the momentum for the Human Genome Project without both the success in finding the CF gene and the fact that it was so darn hard that nobody thought we could do that,” Collins said. “We had to have a foundational understanding of the genome if this was going to be scalable to other conditions.”
Connecting the dots
Welsh led the team that elucidated the role of the CFTR protein—the product of the CFTRgene—as the chemical transporter that allows chloride to move in and out of cells. Welsh demonstrated how the CF gene mutations cause cellular malfunction and lead to the range of symptoms seen in the disease. These insights provided the rationale for the subsequent quest toward targeted therapies that repair the function of the aberrant protein.
The impetus for Welsh’s discoveries came in the form of a fax. Welsh recalled standing by a fax machine in August 1989 when a facsimile copy of the first in the Collins-Tsui trio of seminal papers rolled out.
Leafing through the pages, one question loomed large: Could restoring CFTR in cells lacking the protein, in fact, restore these cells’ ability to move chloride in and out?
Welsh knew right there and then he had to take a sabbatical to find out.
“I took that paper and looked at those sequences and pasted them on the back of every lab notebook I had,” Welsh said.
In a critical proof-of-principle demonstration, Welsh showed that restoring the presence of CFTR in epithelial cells lacking the protein rendered them capable of transporting chloride. His work showed that CFTR was, in fact, the chloride channel responsible for the chemical’s movement in and out of cells. Welsh’s work connected the dots between gene mutations in CF and the manifestations of the disease. Further work by Welsh and team demonstrated that malfunction in CFTR can arise from several different perturbations in the cell.
The inevitable next question became: Can a malfunctioning CFTR protein be repaired?
Fixing the protein
Building on Welsh’s discoveries, a team led by Negulescu initiated a 20-plus year quest to identify compounds that modulate the function of the CFTR protein. This work led to the development of the only CF medications available today that correct the underlying protein defect responsible for disease symptoms and restore cells’ ability to transport chloride.
Negulescu recalled getting a fateful phone call in 1998 from Robert Beall, president of the Cystic Fibrosis Foundation. Already an established player in the fields of basic discovery and clinical care of CF, the foundation had devised a bold new strategy to stimulate translational work—invest research dollars in industry, which traditionally shies from orphan diseases such as CF.
At the time, Negulescu was at Aurora, a small biotech in San Diego later acquired by Boston-based Vertex. Aurora was an early adopter of high-throughput drug screening—a technique used to rapidly sift through hundreds of thousands, even millions, of chemical compounds looking for potential medicine “hits.” Today, this is a common approach, but in 1998 it was deemed cutting-edge.
On the phone that day, Beall was persistent. He implored Negulescu to conduct high-throughput screening for candidate compounds for CF.
“I said, we can try, and that got us started,” Negulescu recalled. “It changed our lives, and it changed the lives of many people in this room and many others across the country and the world. I’ll never forget that phone call.”
Negulescu said the team’s goal became crystal clear—find a pill to be taken by mouth that would treat not only the lungs but all of the organs affected by CF.
Welsh’s work revealed that depending on the specific subtype of genetic mutation, a patient could have either a reduced amount or a reduced function of CFTR. Building on these insights, Negulescu’s group focused on developing two classes of medication: CFTR correctors, which enable the processing and movement of the CFTR protein and increase its amount and presence on the cell surface, and CFTR potentiators, which boost the function and activity of CFTR once it is present in sufficient amounts.
The first small-molecule drug for CF, ivacaftor, a protein potentiator, was approved by the FDA in 2012.
In the initial clinical trial, involving 20 patients—reported in The New England Journal of Medicine—the drug performed beyond expectations. It did not merely restore CFTR function. It did not merely slow the rate of progression of lung disease. It led to an acute improvement in lung function in a span of 14 days. Long-term follow-up has demonstrated that the drug also slows overall disease progression.
“Even though this was eight years ago, I am still as excited as I was the first day because it opened the door,” Negulescu said. “It was the first study that showed we could correct the CFTR function in vivo with a small molecule.”
Two dual-drug combination treatments followed, expanding therapeutic benefits to patients with additional gene mutations. The current CFTR-modulating drugs address the genetic mutations seen in more than half of all CF patients. If proven effective, a triple-compound therapy that is now in clinical testing could extend therapeutic benefit to more than 90 percent of people with CF, and do so within a year or two, Negulescu said.
To clinic!
Ramsey, a pediatric pulmonologist and an HMS alumna, was the architect of the clinical trial network and seminal studies that led to the approval of the first, and subsequent, small-molecule treatments in current use and played a critical role in ensuring the translation of these therapies from lab to clinic.
“I’ve had the honor to witness this journey from bench to bedside and to understand the challenges and joys of being a clinical translational researcher,” Ramsey said.
Ramsey recalled the growing anxiety she felt when she attended meetings with Negulescu’s team. She witnessed the progress made by high-throughput screening for candidate CF compounds.
“I had this vision that we were running a race, and the clinicians would be the last leg of the race,” Ramsey said. “My big fear was that we would get the drug, but we would be unable to prove it’s effective and safe and it wouldn’t get to patients.”
Key to the success of the clinical trials, Ramsey said, was the ability to genotype the entire CF population to ensure that the right CFTR drug was given to the right person depending on their precise mutation. Presciently, in 1989, Tsui had launched a global gene database where every clinician caring for a CF patient could submit DNA samples, Ramsey said. That database remains active.
One of the challenges during clinical trial design faced by Ramsey and colleagues was linking patients’ laboratory biomarkers to actual clinical outcomes. In other words, researchers had to determine the most accurate yardstick to measure whether the drug was working. Was lung function the best indicator? Or was it the amount of chloride excreted in sweat?
In the end, the researchers chose sweat chloride as the most reliable clinical indicator that robustly correlates with CFTR function. The therapeutic goal that would determine the efficacy of a drug was to bring down the level of chloride in sweat.
In the first cohort of CF patients—160—ivacaftor brought down chloride levels dramatically within the first two months of treatment and remained stable over 12 months, Ramsey said. Participants reached levels well below the detectable cutoff and diagnostic threshold for CF. Their lung function improved significantly as well, Ramsey said.
“It was wonderful to see these numbers, but I’d like to share a personal story with my patient Rick Cissna,” she said.
Cissna was Ramsey’s very first patient when she started her pediatric CF clinic. Cissna stayed with her clinic until he reached adulthood in 1984. The CF gene would not be discovered for another five years.
Ramsey lost touch with Cissna for 30 years. In 2012, after ivacaftor’s approval, the two reconnected. Over the years, Cissna had become homebound, she recalled. He was using intermittent oxygen therapy due to poor lung function. He was unable to exercise. Within a month of starting ivacaftor, he was able to play soccer with his two children and went back to work full time as a teacher, Ramsey said.
“This is the joy of being a translational researcher—to actually see how a drug is changing patients’ lives,” Ramsey said.
The CF story: A blueprint for success
A recurrent theme of the symposium was the unprecedented level of collaboration not only across disciplines, scientists and institutions, but also among academia, industry and the nonprofit/advocacy sectors.
The success of CF represents a triumph of team work that combined the acumen of academia with the courage of a young biotech company and the drive of a nonprofit organization, Daley said.
“Their story is remarkable and serves as an opportunity for all of us to reflect and to learn, so that we can replicate their success again and again,” Daley added.
While the five honorees were pivotal in this success, they represent a massive international effort that involved a network of researchers from academia, industry and the nonprofit sector totaling 2,857 scientists from 2,516 institutions, according to an analysis published in Cell.
“We are honoring five of the most prominent of these scientists here today,” said keynote speaker Pamela Davis, dean of the school of medicine at Case Western Reserve University, a pediatric pulmonologist and one of the nation’s foremost experts in CF. “They are in fact the prime movers, but you have to remember that it really did take a village to get to the point we are at.”
The journey has been as rewarding as it’s been arduous and long, several of the speakers said. It took 75 years from the first clinical description of the disease and 23 years from the identification of the CF gene to develop the first defect-correcting precision drug.
With the advent of new technologies, however, this translational trajectory promises to become much shorter, Davis said.
For example, identifying a disease gene in the 1980s took many years, even decades. Today, it can be done in a matter of days or weeks. Creating disease models took years. Now it takes months.
Screening candidate drug compounds was virtually impossible in the 1980s. Today, researchers can test thousands, even millions, of drugs, in a matter of months. The next frontier in that journey will be the use of gene therapy and gene editing to cure CF.
The lessons learned from the CF story, she added, can illuminate approaches for other conditions, Davis said.
“I think there’s a real opportunity to learn from CF and take our lessons to other genetic diseases, and accelerate progress for them. I think the future is here. I just think it’s not widely distributed yet.”
Even though the Warren Alpert Prize recognizes individual scientists, this year, the Warren Alpert Foundation and HMS gave special recognition to the Cystic Fibrosis Foundation for its catalytic support in the early-stage research, in both the basic and the translational science that ensued. In doing so, the foundation played a transformative role and propelled forward the work that culminated in the development of small-molecule therapies.
To date, the foundation has awarded more than $4 million to 64 scientists. Since the award’s inception in 1987, 10 honorees have also received a Nobel Prize. Most recently, 2017 award winners Jim Allison and Tasuku Honjo received the 2018 Nobel Prize in Physiology or Medicine for their for discoveries in cancer immunology.
Negulescu, Ramsey, Tsui and Welsh shared $500,000 in prize money. As a federal employee, Collins declined the cash component of the award.


