HIV is a master at evading the immune system, using a variety of methods to prevent the body from being able to find and kill it. The vast majority of people living with HIV require daily medication to suppress the virus and therefore prevent the development of AIDS.
But for a small subset of people, this battle between the immune system and the virus looks quite different. Known as controllers, they have immune systems that can suppress the virus without any need for medication.
Whereas most controllers can suppress the virus indefinitely, some eventually lose control over the virus and require medication to achieve viral suppression.
In a paper published Sept. 7 in Immunity, Harvard Medical School researchers at the Ragon Institute of MGH, MIT, and Harvard reported that, in these cases, control is lost after a type of immune cell, called a cytotoxic T cell, loses the ability to proliferate and kill HIV-infected cells.
In order to find these differences, the researchers, led by David Collins, HMS research fellow in medicine at Massachusetts General Hospital, compared samples collected over several years from cohorts of HIV controllers at the Ragon Institute and the University of California at San Francisco.
The study included 17 subjects with aborted control and 17 with durable control, whose immune systems continued to suppress HIV over years of observation.
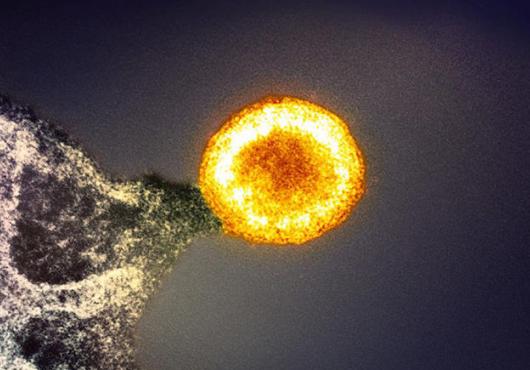
In a successful immune response, cytotoxic T cells recognize small pieces of HIV, called antigens, which are found on the surface of infected cells. The T cells then kill the infected cells, destroying the virus inside.
If mutations in HIV were changing the antigens, the T cells may no longer be able to recognize them. Therefore, the most likely difference, the team thought, might be in the antigens themselves.
Comparing antigens
First, the team compared what type of antigens were presented by infected cells. Co-author Gaurav Gaiha, HMS assistant professor of medicine at Mass General, had previously shown that in controllers cytotoxic T cells often recognize HIV antigens that are unlikely to mutate.
When the team compared the two groups, they found that both sets of T cells responded to the same types of unlikely-to-mutate antigens, meaning they were starting from similar immune responses.
Working with co-author Todd Allen, HMS professor of medicine at Mass General, and his team, the researchers next sequenced HIV from before and after loss of control, looking for mutations that could cause changes in the antigens the T cells recognized.
Even though HIV constantly mutates, within their cohort of 17 patients, they found only one mutation that allowed the antigen to escape T cell recognition.
Mutational escape wasn’t the answer, either. There was also no evidence of superinfection, the term for contracting a second, separate HIV infection, another theory that had been suggested in case studies.
The difference, therefore, was likely in the immune response itself, instead of being driven by the virus.
The team looked more closely at the HIV-specific T cells in both groups, focusing on how well the T cells could perform their various functions.
Cytotoxic T cells have two important functions when they encounter a cell presenting an HIV antigen. The first is their ability to kill infected cells by systematically rupturing them, called cytolysis.
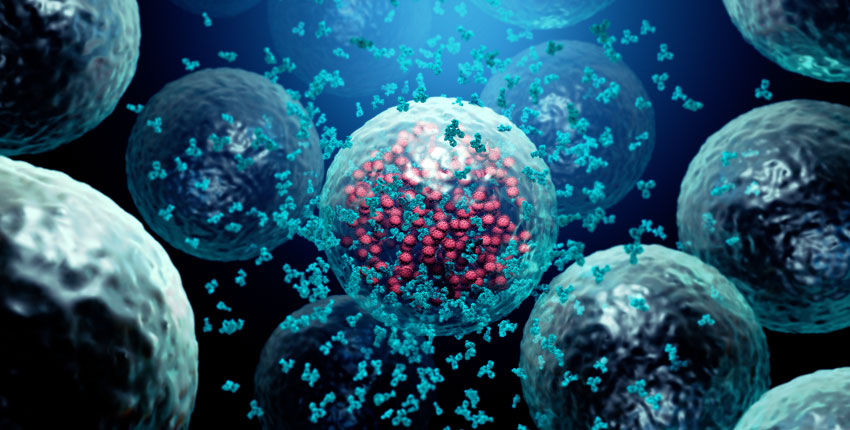
The second function is their proliferative function: creating more HIV-specific T cells that can then hunt down and kill other infected cells.
In progressors—people with HIV who cannot control the virus naturally and who require medication to suppress it—T cells quickly become desensitized to the HIV antigens and stop responding to them, a state known as T cell exhaustion.
T cell dysfunction
Researchers thought perhaps a similar process was happening to T cells when control was lost, but they found no such evidence. With the loss of control came a clear dysfunction of the T cells—the inability to kill cells infected by HIV—but it was a different type of dysfunction than was observed in most infections.
In the group of people who lost control of HIV, there was a measurable decrease in the proliferative and cytolytic ability of the T cells seen in samples taken before the loss of control, sometimes even years before.
In addition, this dysfunction was only seen in response to HIV; the T cells were able to respond properly to other viral antigens. The researchers had thought that T cell dysfunction would come after or during loss of control, but here, the evidence shows that T cell dysfunction actually precedes it.
“Loss of proliferation was the most consistent predictor of aborted control in our study,” said Collins. “In these cases, HIV-specific T cells gradually lost their ability to proliferate and become cytolytic, sometimes years before control was lost.”
In analyses led by computational biologist and second author Jonathan Urbach of the Ragon Institute, the team next compared the genes expressed by the T cells in the two groups and found another important difference, one linked to their earlier observations.
The T cells in the loss of control group had increased expression of KLF2, a gene that, when expressed at high levels, impairs the ability of T cells to proliferate.
“This study shows that loss of control is notably different from the inability to control the virus found in the canonical immune response to HIV,” said Ragon Institute director Bruce Walker, the paper’s senior author.
“It further underlines the importance of a functional, effective T cell response to HIV in natural immune control of the virus. And with each secret HIV reveals comes an opportunity for us to use that knowledge to our advantage,” said Walker, who is also the Phillip T. and Susan M. Ragon Professor of Medicine at HMS and Mass General.
That knowledge might ultimately help researchers work towards treatments and vaccines that could train progressors’ immune systems. Further work remains to understanding why T cells become dysfunctional in some people and not in others.
The study was supported by the Howard Hughes Medical Institute, Bill and Melinda Gates Foundation, Mark and Lisa Schwartz Foundation, Phillip and Susan Ragon Foundation, National Institutes of Health, Fondo de Investigación Sanitaria, Spanish AIDS Research Network, CFAR Network of Integrated Clinical Systems, Delaney AIDS Research Enterprise, amfAR Institute for HIV Cure Research, UCSF/Gladstone Institute of Virology and Immunology Center for AIDS Research, and Harvard University Center for AIDS Research.