The latest organ-on-a-chip from Harvard’s Wyss Institute for Biologically Inspired Engineering reproduces the structure, functions and cellular makeup of bone marrow, a complex tissue that until now could be studied intact only in living animals, Wyss researchers report in the May 4, 2014, online issue of Nature Methods. The device, dubbed “bone marrow-on-a-chip,” gives scientists a much-needed new tool to test the effects of new drugs and toxic agents on whole bone marrow.
Specifically, the device could be used to develop safe and effective strategies to prevent or treat radiation’s lethal effects on bone marrow without resorting to animal testing, a challenge that is being pursued at the Wyss with funding support from the U.S. Food and Drug Administration. In an initial test, the engineered bone marrow, like human marrow, withered in response to radiation unless a drug known to prevent radiation poisoning was present.
The bone marrow-on-a-chip could also be used in the future to maintain a cancer patient’s own marrow temporarily while he or she underwent marrow-damaging treatments such as radiation therapy or high-dose chemotherapy.
“Bone marrow is an incredibly complex organ that is responsible for producing all of the blood cell types of our body, and our bone marrow chips are able to recapitulate this complexity in its entirety and maintain it in a functional form in vitro,” said Don Ingber, founding director of the Wyss Institute, Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital, professor of bioengineering at the Harvard School of Engineering and Applied Sciences, and senior author of the paper.
Ingber leads a large effort to develop human organs-on-chips–small microfluidic devices that mimic the physiology of living organs. So far, Wyss teams have built lung, heart, kidney and gut chips that reproduce key aspects of organ function, and they have more organs-on-chips in the works. The technology has been recognized internationally for its potential to replace animal testing of new drugs and environmental toxins and as a new way for scientists to model human disease.
To build organ chips in the past, Wyss teams have combined multiple types of cells from an organ on a microfluidic chip while steadily supplying nutrients, removing waste and applying mechanical forces the tissues would face in the body. But bone marrow is so complex that they needed a new approach to mimic organ function.
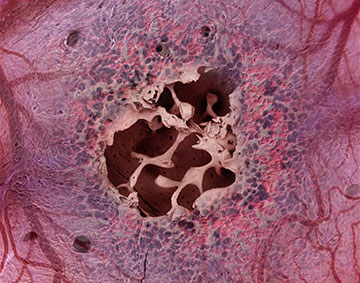
This complexity arises because bone marrow has an integral relationship with bone. Marrow sits inside trabecular bone—a solid-looking type of bone with a porous, honeycombed interior. Throughout the honeycomb, conditions vary: Some areas are warmer, some cooler; some are oxygen-rich, others oxygen-starved—and the dozen or so cell types each have their own preferred spots. To add complexity, bone marrow cells communicate with each other by secreting and sensing a variety of biomolecules, which act locally to tell them whether to live, die, specialize or multiply.
Rather than trying to reproduce such a complex structure cell by cell, the researchers enlisted mice to do it.
“We figured, why not allow Mother Nature to help us build what she already knows how to build,” said Catherine Spina, an MD-PhD candidate at Boston University, a researcher at the Wyss, and co-lead author of the paper.
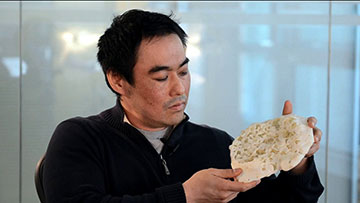
Specifically, Spina and Yu-suke Torisawa, a postdoctoral fellow at the Wyss, packed dried bone powder into an open ring-shaped mold the size of a coin battery and implanted the mold under the skin on the animal’s back.
After eight weeks, they surgically removed the disk-shaped bone that had formed in the mold and examined it with a specialized CAT scanner. The scan showed a honeycomb-like structure that looked identical to natural trabecular bone.
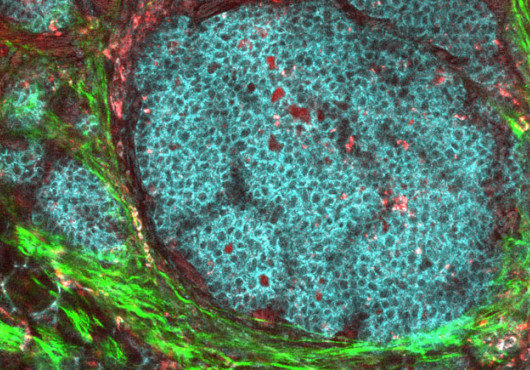
The marrow looked like the real thing as well. When they stained the tissue and examined it under a microscope, the marrow was packed with blood cells, just like marrow from a living mouse. And when the researchers sorted the bone marrow cells by type and tallied their numbers, the mix of different types of blood and immune cells in the engineered bone marrow was identical to that in a mouse thighbone.
To sustain the engineered bone marrow outside of a living animal, the researchers surgically removed the engineered bone from mice, then placed it in a microfluidic device that steadily supplied nutrients and removed waste to mimic the circulation the tissue would experience in the body.
Marrow in the device remained healthy for up to one week—long enough, typically, to test the toxicity and effectiveness of a new drug.
The device also passed an initial test of its drug-testing capabilities. Like marrow from live mice, this engineered marrow was also susceptible to radiation, but an FDA-approved drug that protects irradiated patients also protects the marrow on the chip.
In the future, researchers could potentially grow human bone marrow in immune-deficient mice. “This could be developed into an easy-to-use screening-based system that’s personalized for individual patients,” said coauthor James Collins, a core faculty member at the Wyss and the William F. Warren Distinguished Professor at Boston University, where he leads the Center of Synthetic Biology.
Bone marrow-on-a-chip could also generate blood cells, which could circulate in an artificial circulatory system to supply a network of other organs-on-chips. The Defense Agency Advanced Research Projects Agency is also currently providing funds to the Wyss to develop an interconnected network of 10 organs on chips to study complex human physiology outside the body.
The work was funded by the U.S. Food and Drug Administration, DARPA and the Wyss Institute for Biologically Inspired Engineering at Harvard University.
Adapted from a Wyss Institute news release.