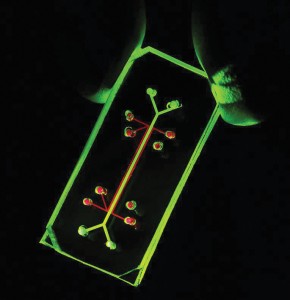
Researchers from the Wyss Institute for Biologically Inspired Engineering at Harvard University, HMS and Children’s Hospital Boston have created a device on a microchip that mimics a living, breathing human lung. About the size of a rubber eraser, it makes use of human lung and blood vessel cells.
Because the lung device is translucent, it provides a window into the inner-workings of the human lung without the need to invade a living body. It has the potential to be a valuable tool for testing the effects of environmental toxins, absorption of aerosolized therapeutics and the safety and efficacy of new drugs. Such a tool may help accelerate pharmaceutical development by reducing the reliance on current models, in which testing a single substance can cost more than $2 million.

Lung on a chip: Researchers from the Wyss Institute for Biologically Inspired Engineering have created a device that mimics a living, breathing human lung on a microchip.
“The ability of the lung-on-a-chip device to predict absorption of airborne nanoparticles and mimic the inflammatory response triggered by microbial pathogens provides proof of principle for the concept that organs on chips could replace many animal studies in the future,” said Donald Ingber, senior author on the study and founding director of Harvard’s Wyss Institute.
The paper appears in the June 25 issue of Science.
Room to BreatheUntil now, tissue-engineered microsystems have been limited either mechanically or biologically, said Ingber, who is also the Judah Folkman professor of vascular biology at HMS and CHB. “We really can’t understand how biology works unless we put it in the physical context of real living cells, tissues and organs.”
With every human breath, air enters the lungs, fills microscopic air sacs called alveoli and transfers oxygen into the bloodstream through a thin, flexible, permeable membrane of lung cells. It is this membrane—a three-layered interface of lung cells, a permeable extracellular matrix and capillary blood vessel cells—that does the lung’s heavy lifting. What’s more, this lung–blood interface recognizes invaders such as inhaled bacteria or toxins and activates an immune response.
The lung-on-a-chip device takes a new approach to tissue engineering by placing two layers of living tissue—the lining of the lung’s air sacs and the blood vessels that surround them— across a porous, flexible boundary. Air is delivered to the lung-lining cells, a rich culture medium flows in the capillary channel to mimic blood, and cyclic mechanical stretching mimics breathing. The device was created using a novel microfabrication strategy that uses clear rubbery materials. The technique was pioneered by another Wyss core faculty member, George Whitesides, the Woodford L. and Ann A. Flowers University professor at Harvard University.
“We were inspired by how breathing works in the human lung through the creation of a vacuum that is created when our chest expands, which sucks air into the lung and causes the air sac walls to stretch,” said first author Dan Huh, a Wyss technology development fellow at the institute. “Our use of a vacuum to mimic this in our microengineered system was based on design principles from nature.”

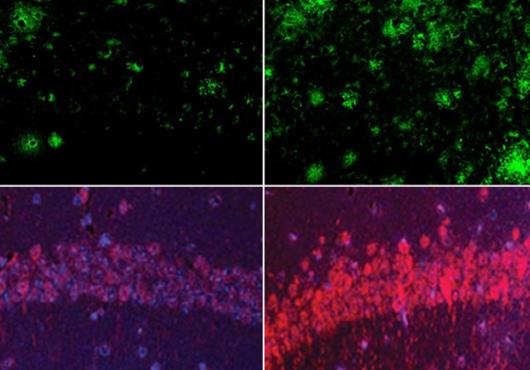
To determine how well the device replicates the natural responses of living lungs to stimuli, the researchers tested its response to inhaled, living E. coli bacteria. They introduced bacteria into the air channel on the lung side of the device and, at the same time, flowed white blood cells through the channel on the blood vessel side. The lung cells detected the bacteria and, through the porous membrane, activated the blood vessel cells, which in turn triggered an immune response that ultimately caused the white blood cells to move to the air chamber and destroy the bacteria.
“The ability to recreate both the mechanical and biological sides of the in vivo coin is an exciting innovation,” said Rustem Ismagilov, professor of chemistry at the University of Chicago, who specializes in biochemical microfluidic systems.
The team followed this experiment with a “real-world application of the device,” said Huh. They introduced a variety of nanoscaled particles into the air sac channel. Some of these particles exist in commercial products; others are found in air and water pollution. Several types of these nanoparticles entered the lung cells and caused the cells to overproduce free radicals and to induce inflammation. Many of the particles passed through the model lung into the blood channel, and the investigators discovered that mechanical breathing greatly enhanced nanoparticle absorption. Benjamin Matthews, HMS assistant professor of pediatrics in the Vascular Biology Program at Children’s, verified these new findings in mice.
“Most importantly, we learned from this model that the act of breathing increases nanoparticle absorption and that it also plays an important role in inducing the toxicity of these nanoparticles,” Huh said.
Organs on Chips“This lung on a chip is neat and merges a number of technologies in an innovative way,” said Robert Langer, the David H. Koch institute professor at MIT. “I think it should be useful in testing the safety of different substances on the lung, and I can also imagine other related applications, such as in research into how the lung functions.” In addition, the device opens the door to creating lung-on-a-chip systems using a patient’s own cells for testing individualized therapies.
According to Ismagilov, it is too early to predict how successful this field of research will be. Still, “the potential to use human cells while recapitulating the complex mechanical features and chemical microenvironments of an organ could provide a truly revolutionary paradigm shift in drug discovery,” he said.
The investigators have not yet shown the system’s capability to mimic gas exchange between the air sac and bloodstream, a key function of the lungs, but, Huh said, they are exploring this now.
The Wyss Institute team is also working to build other organ models, such as a gut on a chip, as well as bone marrow and even cancer models. Further, they are exploring the potential for combining organ systems.
Ingber, for example, is collaborating with Kevin Kit Parker, associate professor at Harvard University’s School of Engineering and Applied Sciences and another Wyss core faculty member, who has created a beating heart on a chip. They hope to link the breathing lung on a chip to the beating heart on a chip. The engineered organ combination could be used to test inhaled drugs and to identify new and more effective therapeutics that do not cause adverse cardiac side effects.
For more information, students may contact Don Ingber at don.ingber@wyss.harvard.edu.
Conflict Disclosure: The authors declare no conflicts of interest.
Funding Sources: The National Institutes of Health, the American Heart Association and the Wyss Institute for Biologically Inspired Engineering at Harvard University; the authors are solely responsible for the content of this work.