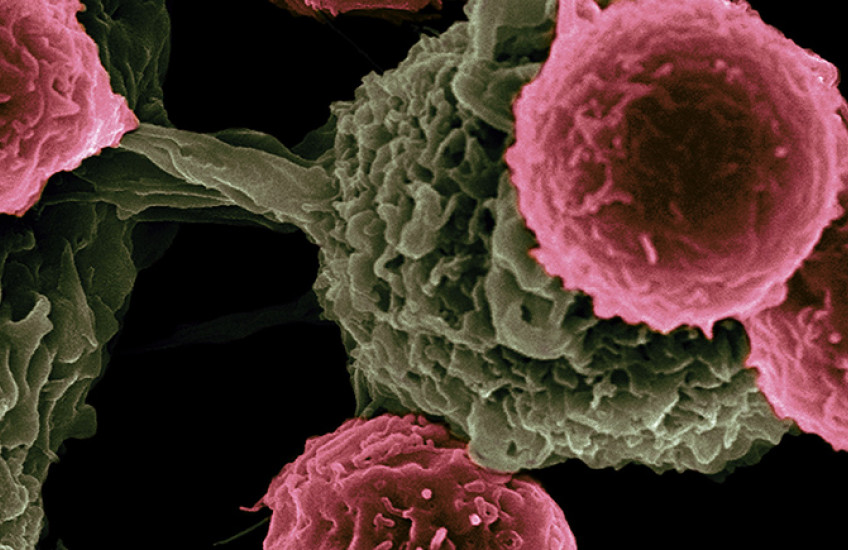
Successful immunotherapy for cancer involves activating a person’s own T cells to identify telltale proteins called antigens on the surface of a tumor and attack it. But some tumors have a trick: They hide themselves from the immune system by preventing their antigens from being displayed.
A team led by Harvard Medical School researchers at Boston Children’s Hospital has now found a way around this defense in mice.
The findings suggest a strategy for developing add-on treatments that make cancer immunotherapies more effective.
The key lies in a protein called prosaposin, the team reported in Science.
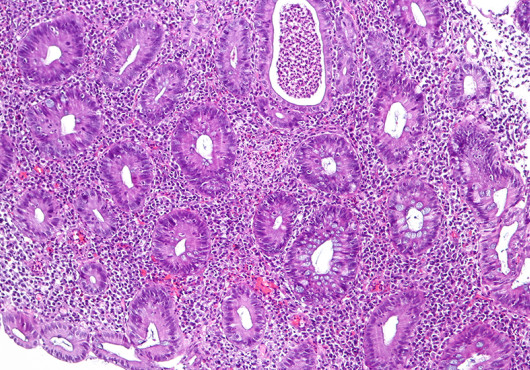
Tumor tissue contains a large percentage of dying cells that shed little capsules, or vesicles, containing the tumor antigens. Immune cells called dendritic cells absorb these vesicles, process the antigens, and sprout pieces of the antigens on their surface, which teaches T cells to recognize and attack the antigens.
The researchers found that without prosaposin, dendritic cells can’t break down the vesicles and present the tumor antigens to the immune system as a teaching tool.
Specifically, the dendritic cells need proteins called saposins that form from prosaposin, the team discovered.
“We found that saposins are needed to digest these vesicles and free the tumor antigen for display to the immune system,” explained senior author Florian Winau, HMS associate professor of pediatrics in the Program in Cellular and Molecular Medicine at Boston Children’s.
Getting tumor antigens out of hiding
Winau and colleagues found that tumors hide their antigens from the immune system by loading prosaposin with chains of sugar molecules. This makes dendritic cells secrete the prosaposin, depleting their supply of saposins. The cells then can’t digest vesicles and release the tumor antigens inside.
The team’s next step was to try adding prosaposin back.
In a mouse model of the skin cancer melanoma, the team gave an IV of prosaposin coupled to an antibody that homes in on dendritic cells.
The treatment enabled the animals’ immune systems to once again detect the tumor antigens and activate T cells.
When the researchers combined prosaposin with immune checkpoint inhibitor drugs, they saw reduced tumor growth.
Further studies are needed to confirm whether prosaposin-based treatment would work in humans.
Winau and colleagues have filed for a patent on the technology. Working with an industry partner, they have devised a targeted system to deliver prosaposin and hope to develop a candidate drug to test in human clinical trials.
In a separate project, they’re working on a diagnostic test that would detect sugar-coated prosaposin in human blood. The goal is to indicate when a person’s tumor-antigen presentation is impaired and the tumor is escaping immune attack, meriting a change of treatment.
Authorship, funding, disclosures
Pankaj Sharma, Xiaolong Zhang, and Kevin Ly were co-first authors on the paper. Additional authors are Ji Hyung Kim, Qi Wan, Jessica Kim, Mumeng Lou, Lisa Kain, and Luc Teyton.
The study was funded by the National Institutes of Health (grant R01AI136939).
Winau and Sharma are listed as inventors on a patent application filed by Boston Children’s Hospital (provisional application no. 63/350,734), which covers the use of pSAP in cancer therapy. The authors declare no conflict of financial interests.