As more patients choose to spend their final days and weeks in hospice care rather than a hospital, the hope has been that the use of intensive and costly hospital services would decline.
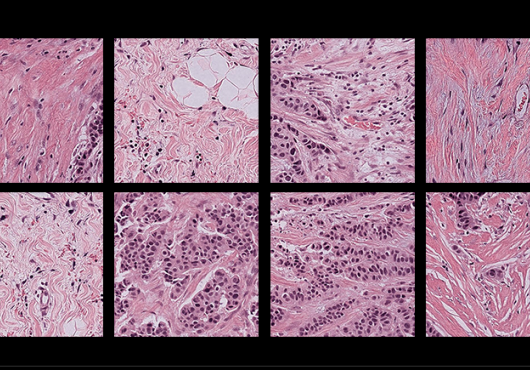
A new study by Harvard Medical School and Dana-Farber Cancer Institute researchers shows that, for one group of terminally ill cancer patients, this is not what is happening, despite efforts to improve the quality of life of patients near the end of life.
The study, which tracked nearly 7,000 older patients with ovarian cancer, found that between 1997 and 2007, patients were more likely to enter a hospice and less likely to die in a hospital.
However, their use of hospital-based services actually increased. These seemingly paradoxical findings, published in the October issue of the Journal of Clinical Oncology, suggest that many patients received aggressive treatments while in the hospital, and resorted to hospice care as an add-on when those treatments failed, the authors wrote.
“There’s a growing awareness that the use of aggressive, expensive medical interventions at the end of life often doesn’t improve patients’ quality of life and may even make it worse,” said Alexi Wright, HMS assistant professor of medicine at Dana-Farber and lead author of the study.
“Hospice care, which focuses on intensive symptom management at home, is an attractive option for many people. But unless people make an end-of-life care plan while they’re healthy—spelling out their preferences in advance—these important decisions are often made for them, or occur in a crisis atmosphere. That may explain why, in this study, we saw an increased use of hospital-based services even as hospice enrollment increased,” said Wright.
The study analyzed the Medicare records of 6,956 women aged 66 or older who were diagnosed with ovarian cancer between 1997 and 2007, and who died of the disease by the end of 2007.
The researchers found that hospice use increased significantly during that period, while hospitalized deaths fell. But they also found significant increases in intensive care unit admissions, hospitalizations, repeated emergency department visits and transitions from one health care facility to another.
During the same time frame, the proportion of patients who were referred to hospice from a hospital inpatient clinic rose. And 70 percent of patients were transferred between medical facilities at least once in the last month of life—with 20 percent experiencing major transitions between care settings within the final three days of life.
The findings paint a hectic picture of elderly terminally ill patients undergoing multiple stressful medical interventions and undergoing transfers between facilities, all before arriving at a hospice, where their stay may be very brief.
“The earlier people can make plans—with their families and physicians—the better they can control the kind of care they receive at the end of life,” said Wright.
“Many people want their final days to be a time of legacy building—a time when they can share or build memories with their loved ones—instead of time spent in hospitals or receiving potentially futile medical interventions. Our study points to the extent to which such planning is still needed,” she said.
The study was supported by grants from the National Cancer Institute, the American Cancer Society, the American Society for Clinical Oncology, the National Palliative Care Research Center and the Gloria Spivak Faculty Advancement Fund.
Adapted from a Dana-Farber news release.