A novel approach to cancer immunotherapy—strategies designed to induce the immune system to attack cancer cells—may provide a new and cost-effective weapon against some of the most deadly tumors, including ovarian cancer and mesothelioma.
Investigators from Harvard Medical School and the Massachusetts General Hospital Vaccine and Immunotherapy Center report in the Journal of Hematology & Oncology that a protein they engineered was able to prolong survival in animal models of both tumors. Their success came from combining a molecule that targets a tumor-cell-surface antigen with another protein that stimulates several immune functions.
“Some approaches to creating cancer vaccines begin by extracting a patient’s own immune cells, priming them with tumor antigens and returning them to the patient, a process that is complex and expensive,” said Mark Poznansky, HMS associate professor of medicine at Mass General. He is director of the hospital’s Vaccine and Immunotherapy Center and senior author of the paper. “Our study describes a very practical, potentially broadly applicable and low-cost approach that could be used by oncologists everywhere, not just in facilities able to harvest and handle patients’ cells.”
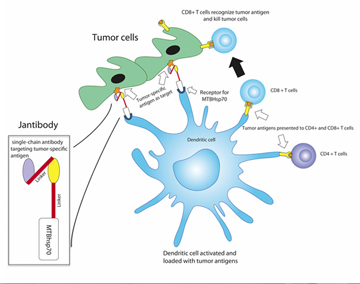
The team’s vaccine would stimulate the patient’s own dendritic cells, a type of immune cell that monitors an organism’s internal environment for the presence of viruses or bacteria. These cells also ingest and digest pathogens they encounter and display antigens from those pathogens on their surfaces to direct the activity of other immune cells. Existing cancer vaccines that use dendritic cells require extracting cells from a patient’s blood, treating them with an engineered protein or nucleic acid that combines tumor antigens with immune-stimulating molecules, and returning the activated dendritic cells to the patient.
The approach developed by the Mass General team starts with the engineered protein, which in this case fuses an antibody fragment targeting a protein called mesothelin—expressed on the surface of mesothelioma, ovarian cancer and pancreatic cancer tumors—to a protein from the tuberculosis bacteria. That fused protein stimulates the activity of dendritic and other immune cells. In this system, the dendritic cells are activated and targeted against tumor cells while remaining inside the patient’s body.
In the animal experiments described in the paper, the MGH team confirmed that their mesothelin-targeting fusion protein binds to mesothelin on either ovarian cancer or mesothelioma cells, activates dendritic cells, and enhances the cells’ processing and presentation of several different tumor antigens, inducing a number of T-cell-based immune responses. In mouse models of both tumors, treatment with the fusion protein significantly slowed tumor growth and extended survival, probably through the activity of cytotoxic CD8 T cells.
“Many patients with advanced cancers don’t have enough functioning immune cells to be harvested to make a vaccine, but our protein can be made in unlimited amounts to work with the immune cells patients have remaining,” explained study co-author Jeffrey Gelfand, HMS clinical professor of medicine at Mass General. “We have created a potentially much less expensive approach to making a therapeutic cancer vaccine that, while targeting a single tumor antigen, generates an immune response against multiple antigens. Now if we can combine this with newly described ways to remove the immune system’s ‘brakes’—regulatory functions that normally suppress persistent T-cell activity—the combination could dramatically enhance cancer immunotherapy.”
Poznansky added that the ovarian cancer, pancreatic cancer and mesothelioma tumors that might be treated with the mesothelin-targeting vaccine all have poor survival rates. “Immunotherapy is generally nontoxic, so this vaccine has the potential of safely extending survival and reducing the effects of these tumors, possibly even cutting the risk of recurrence. We believe that this approach could ultimately be used to target any type of cancer and are currently investigating an improved targeting approach using personalized antigens.”
The team recently received a two-year grant from the Department of Defense Congressionally Directed Medical Research Program to continue its research.
Poznansky, Gelfand and their co-authors dedicate the paper to Janet Gelfand, wife of Jeffrey Gelfand, who died of ovarian cancer in 2006 and inspired their investigation. In her honor they have named their tumor-targeting fusion protein Jantibody.
Support for the study includes grants from the Edmund Lynch Jr. Cancer Fund, Arthur Luxenberg Esq., Perry Weitz Esq., the Vaccine and Immunotherapy Center Mesothelioma Research and Resource Program, and the Friends of VIC Fund.
Adapted from a Mass General news release.


