Researchers from Harvard Medical School and the Broad Institute of MIT and Harvard have uncovered unexpectedly complex patterns in the T lymphocyte responses that individual people mount, reflecting environmental influences as well as a genetic component. The study lays the groundwork for further explorations into the relative contributions of genes and their environment on immunological processes, the scientists said, which could illuminate autoimmune disease and its genetic underpinnings.
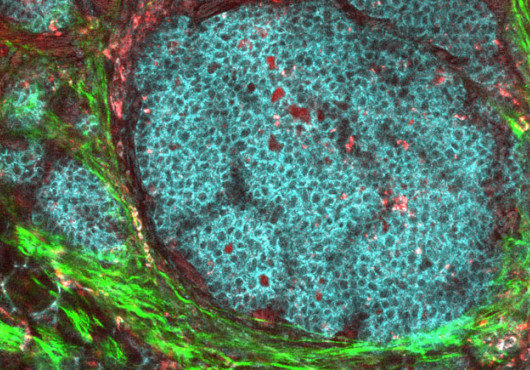
The findings are reported in Science and stem from the ImmVar Project, a wide-ranging analysis of variation in gene expression in the immune system. Christophe Benoist, Morton Grove-Rasmussen Professor of Immunohematology at HMS, and Aviv Regev, a Broad Institute core member, an associate professor at MIT, and Howard Hughes Medical Institute investigator, led the third and final phase, which focused on CD4+ T cells, immune cells that are major players in autoimmune disease.
In this study, after the scientists accounted to the best possible extent for environmental influences and immunological history, they still found that the ancestry of the donor significantly affected T cell responses. “There is a signature of variation in adaptive immune response,” Benoist said. “In general, there is stronger activation of some genes in people of African ancestry, in particular for a type of response in T helper 17 (Th17) cells that tend to protect us from microbes that enter airways or the intestinal tract. Those responses are also highly involved in autoimmune disease.”
“The combination of careful immunological work, high-throughout assays, and sophisticated analytics essential to dissect such a complex system could only have happened within the partnership of the ImmVar consortium, bringing together the expertise of immunologists and clinicians in the Harvard-affiliated hospitals with genomics and computational experts at the Broad and MIT,” Regev said.
In autoimmune diseases such as rheumatoid arthritis, inflammatory bowel disease and multiple sclerosis, immune cells mistakenly attack the body’s own tissues as if they were invaders. In healthy people, the immune system achieves a state of tolerance, quelling defensive measures after a threat has abated.
Scientists have previously identified genes that are important in controlling the autoimmune response, but this is the first time that differences in T cell activation between population groups have been revealed.
In the current study, the scientists analyzed blood samples collected from 348 healthy volunteers representing African, Asian or European ancestry. After the researchers genotyped the samples and isolated CD4+ T cells, the T cells were activated in cell culture to model their response to antigens. A computational analysis measured which genes were turned on or off in the cells from each person.
Activation of autoimmune-associated genes can vary between individuals in a complicated interplay of genes and environment. Each person’s immunological history is written in a constellation of events, from being vaccinated against the measles in childhood to having the flu last winter. Benoist compares it to learning and personality: All the memories you accumulate make you who you are.
In one’s immunological history, “environment” also encompasses the microbial world people inhabit. The hygiene hypothesis holds that people who have encountered more challenges to their immune system—harmful microbes—are less likely to have the runaway response that is the hallmark of autoimmune disease. People who grow up exposed to fewer microbes may have difficulty stopping the immune response when it is no longer needed.
There is a strong inherited component to autoimmune disease, but changing one’s environments is also important, Benoist noted. People who relocate to a new region tend to acquire the frequency of autoimmune disease of where they are going, observational research has reported. For example, he said, there is little autoimmune disease in India, but people of Indian origin who have lived in the US, from an early age have about the same frequency of autoimmune disease as people of European origin who also live in the US.
One possibility is that at least some of this variation may reflect evolutionary adaptations to the pathogens people encountered during human migrations out of Africa 50,000 years ago. A more robust immune response would have been advantageous in sub-Saharan Africa but deleterious at higher latitudes, with fewer microbial pathogens.
“It’s a tantalizing idea, but it’s highly speculative,” Benoist said.
This work was supported by National Institute of General Medical Sciences grant RC2 GM093080, NIH F32 Fellowship (F32 AG043267), HHMI, and a Harry Weaver Neuroscience Scholar Award from the National Multiple Sclerosis Society (JF2138A1).