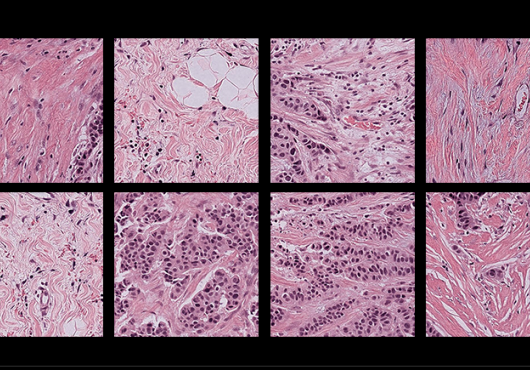
A typical neuroblastoma. Image: Maria Tsokos/National Cancer Institute
Great strides have been made in treating neuroblastoma, the most common cancer in infants and toddlers. However, advanced cases are often fatal, and children who survive often face lifelong physical and intellectual challenges related to their treatment.
A study published online in Nature, led by Harvard Medical School researchers at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, finds that let-7, a microRNA, is central in curbing neuroblastoma.
The study unifies several theories about neuroblastoma and could focus efforts to find a targeted, nontoxic alternative to chemotherapy.
The findings also have implications for other solid tumors in which let-7 is lost, such as Wilms’ tumor (nephroblastoma) and lung, breast, ovarian and cervical cancers, said first author John Powers, HMS research fellow in biological chemistry and molecular pharmacology and a senior scientist in the laboratory of George Q. Daley.
Daley, the Robert A. Stranahan Professor of Pediatrics and Professor of Biological Chemistry and Molecular Pharmacology at HMS and director of the Stem Cell Transplantation Program at Dana-Farber/Boston Children’s, is senior author on the paper.
The let-7 family of microRNAs—bits of genetic code that regulate genes—is known to be involved in both stem-cell differentiation and tumor suppression. Recent research implicated LIN28B, a protein that inhibits let-7 maturation, in neuroblastoma. That made sense: If a cell’s let-7 can’t mature, it can’t differentiate. Instead, it remains stem cell-like and can potentially become cancerous.
But through work on neuroblastoma cells and analysis of patient data, Powers and colleagues found that LIN28B is only one player among several cancer mechanisms, all involving let-7 suppression.
“We’re showing that let-7 inhibition is central to the development of this disease,” said Powers. “So critical, in fact, that neuroblastoma uses at least three distinct ways of eliminating it.”
A unifying theory
Researchers had noticed, for example, that in some cases of neuroblastoma, the oncogene MYCN is hugely amplified—allowing production of many thousands of copies of its mRNA.
“Children with a MYCN-amplification event, which occurs in about 25 percent of cases, have the poorest prognosis,” said Powers. “A big question in neuroblastoma research has been, ‘why does the cancer need so much MYCN mRNA?’”
Powers and colleagues found an answer. They demonstrated that genetic MYCN amplification enables neuroblastomas to sequester let-7, taking it out of circulation.
“MYCN mRNA is expressed at such high levels that it is able to sponge up otherwise functional let-7 and still function as an oncogene,” said Powers.
Similarly, certain chromosome deletions—in the 11q and 3p regions—had been known to be associated with neuroblastoma. Powers and colleagues showed that these lost chunks of DNA are home to multiple let-7 family members.
They also demonstrated that genetic loss of let-7 tracks with poor outcomes. Patients with chromosomal let-7 loss had markedly reduced survival in both MYCN-amplified and non-MYCN-amplified neuroblastoma compared to those with no let-7 loss.
“Genetic loss of let-7 was not widely appreciated in neuroblastoma,” said Powers. “People knew about chromosomal losses and were looking for a tumor suppressor, but they were mainly looking at the protein-coding genes, not microRNAs.”
A pragmatic cancer
Interestingly, in the study’s patient sample, chromosomal loss of let-7 rarely occurred in patients with MYCN amplification. The two cancer-promoting events, both suppressing let-7, were nearly mutually exclusive, meaning most neuroblastomas involved either one or the other, as shown in this Venn diagram.
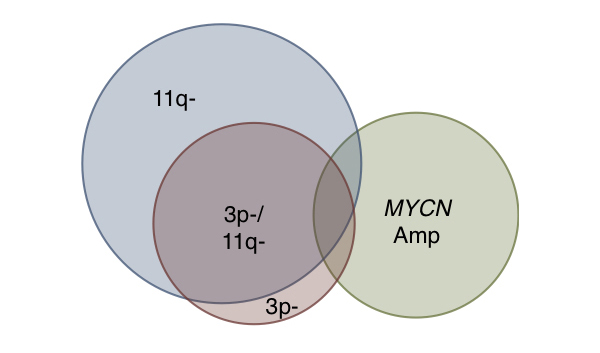
The researchers believe this mutual exclusivity indicates that once a cancer comes up with one weapon, it’s no longer under selective pressure to find another, since to do so would be redundant.
“From the cancer’s point of view, you have to deal with let-7,” said Powers. “If MYCN is not amplified, the tumor instead just loses it genetically. In either case, let-7 is mitigated.”
Likewise, if let-7 is eliminated through chromosomal loss, MYCN amplification becomes unnecessary for the cancer to spread. “Once a tumor has disrupted let-7 genetically, it doesn’t need to sponge let-7, so it doesn’t need to amplify MYCN.”
Precision medicine for neuroblastoma?
The team’s findings, if replicated in a larger number of patient samples, could help establish genetic typing of neuroblastomas, predicting disease severity based on LIN28B levels, genetic loss of let-7 and MYCN amplification. This could potentially guide a precision medicine approach, as happened with medulloblastoma.
As for treatment strategies, Powers believes that restoring let-7 could provide a low-toxicity approach to neuroblastoma and other cancers in which let-7 is lost. Let-7 itself could potentially be a drug, if the challenges of delivery—common to all RNA therapeutics—can be overcome.
Powers wants to work on this challenge. “If we can master let-7, then we could have a less toxic way to treat the disease,” he said. “Then we have the chance to really help those kids.”
The study was supported by the National Institutes of Health (R01GM107536, T32GM007753), Alex’s Lemonade Stand Foundation, the Ellison Medical Foundation and the Howard Hughes Medical Institute.
Adapted from a post on Vector, the research and clinical innovation blog at Boston Children’s.