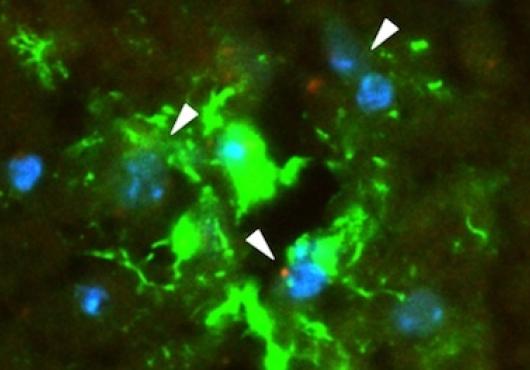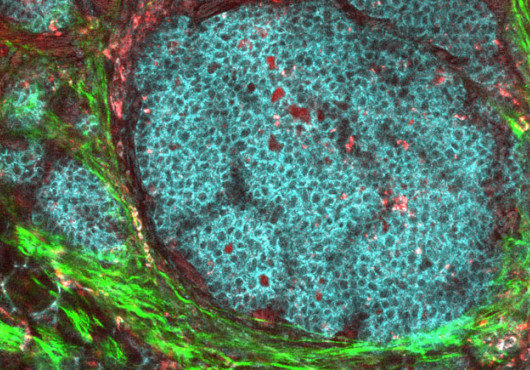
Without a blood supply, a tumor can remain dormant and harmless. But new blood vessel growth from an existing vessel, a process called angiogenesis, is a hallmark of both benign and malignant tumors. During angiogenesis, blood vessels invade tumors and activate them, fueling their growth.
Now, Marsha Moses, the Julia Dyckman Andrus Professor of Surgery at Harvard Medical School and Boston Children’s Hospital, and members of her laboratory have revealed that a specialized imaging system can detect changes in cell behaviors. These changes predict when tumors are leaving a state of dormancy and becoming more likely to grow.
“Can we revert an activated tumor back to its dormant state?” asked Peng Guo, a researcher in the Moses lab, an instructor in surgery at HMS and co-first author of the paper. “The ultimate dream would be to detect when that ‘angiogenic switch’ has flipped and start treatment with nontoxic therapies as soon as possible.”
Until now, methods to identify this switch have been time- and labor-intensive and require expensive reagents and instrumentation.
“We wanted to conduct a visual, economical and quantitative analysis of tumor cells to determine whether or not we could distinguish between dormant and active states,” said Moses, senior author of the paper and director of the Vascular Biology Program at Boston Children’s.
The findings were published in the Journal of the International Society for Advancement of Cytometry.
A new movement in tumor monitoring?
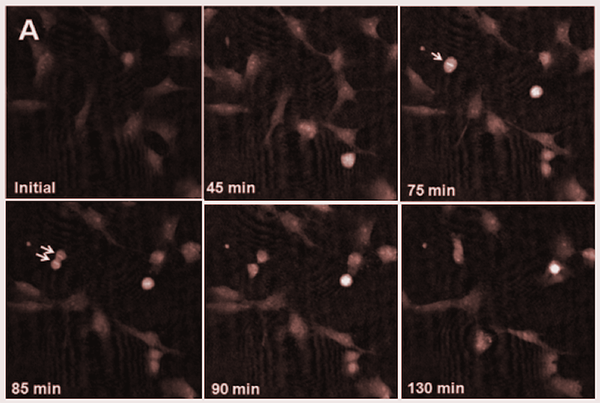
Moses and her team turned to quantitative phase imaging, or QPI. They placed wells of cell cultures underneath a microscope and recorded them in time-lapse. From these images, taken every five minutes over a period of 48 hours, the team did a pixel-by-pixel analysis of the cells’ migration, motility, thickness, volume, proliferation rate and several other factors.
“Using cancer cells, we discovered that we could, in fact, identify changes in cells’ movements that are associated with a tumor’s escape from dormancy,” said Moses.
“We found that angiogenic cells have significantly greater thicknesses, smaller cell areas and higher motility speeds than dormant cells,” said Jing Huang, a researcher in the Moses lab and co-first author of the paper.
“Using cancer cells, we discovered that we could, in fact, identify changes in cells’ movements that are associated with a tumor’s escape from dormancy.” —Marsha Moses
Although still far away from being ready for the clinic, QPI presents a novel method for continuously, efficiently and noninvasively monitoring tumor cells for activation. Moses and her team envision that QPI, in combination with clinical biomarker staining, could one day be used to characterize the percentage of angiogenic and nonangiogenic cells in a given tumor.
“Our hope is that one day, this technology can provide useful clinical information that could be used to guide personalized therapies based on someone’s precise tumor phenotype,” said Huang.
“We are committed to understanding the mechanisms underlying tumor dormancy and leveraging that data in innovative ways, with the eventual goal of making maximum clinical impact,” said Moses.
This study was supported by the Breast Cancer Research Foundation and the Advanced Medical Research Foundation.
Adapted from a post on Vector, the Boston Children’s clinical and research innovation blog.