Up to 80 percent of people with long-standing type 1 diabetes develop gastrointestinal symptoms—abdominal pain, bloating, nausea, vomiting, diarrhea, constipation and fecal incontinence—that severely diminish quality of life.
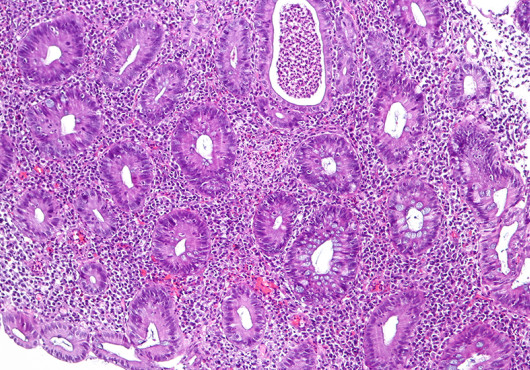
Recent evidence suggests that this condition, known as diabetic enteropathy, results from damage to the intestinal lining, but the details beyond that have been unclear.
A study in this week’s Cell Stem Cell led by Paolo Fiorina, Harvard Medical School assistant professor of pediatrics at Boston Children’s Hospital, now provides some answers. It demonstrates how diabetes can lead to destruction of the stem cells that maintain the intestinal lining, and identifies a potential drug that could protect these stem cells and prevent or treat diabetic enteropathy.
Fiorina and colleagues began by studying 60 patients with long-standing type 1 diabetes. Through proteomic analysis of the patients’ blood, they discovered that a hormone called insulin-like growth factor binding protein 3 (IGFBP3) was strikingly elevated—levels were almost five times those in 20 healthy controls.
Levels of the hormone corresponded with GI symptom severity and colonic stem cell abnormalities. It also rose dramatically in correspondence with patients’ blood sugar levels.
The researchers believe that this spike in IGFBP3, which they dubbed enterostaminine, represents the body’s effort to control diabetes.
“Everyone has enterostaminine, but in people with hyperglycemia, the liver makes more of it,” said Fiorina. “We think that the liver senses the high blood glucose level and makes more of this hormone to try to reduce glucose absorption in the intestine.”
A recombinant drug?
What does enterostaminine do?
Turning to a mouse model of diabetes, Fiorina and colleagues showed that it binds to a receptor in the intestines called TMEM219 and disrupts intestinal stem cell function.
TMEM219 also provided the clue to countering the damage. When Fiorina and colleagues cloned a little piece of it and gave it to the mice, it acted like a sponge, soaking up the circulating enterostaminine and allowing healthy stem cell function to resume.
Paolo Fiorina describes the significance of his team’s findings. Video: Cell PressThe TMEM219-derived protein drug, called ecto-TMEM219, hasn’t yet been tested in diabetes patients. However, patients who had kidney-pancreas transplantation, which restores normal blood glucose levels, saw their enterostaminine levels and colonic stem cell function normalize while their GI symptoms diminished.
Fiorina and colleagues are now doing further tests on the engineered drug to see if it could prevent or treat diabetic enteropathy. They are also testing ways to stop liver cells from producing so much enterostaminine to begin with.
Stem cell therapy without cells
Scientifically, the findings represent one of the first known instances of a hormone controlling stem cell production. They suggest that stem cells’ regenerative qualities can be exploited without having to actually manipulate and deliver cells or figure out how to prevent foreign cells from being destroyed by the immune system.
“If you have hormones like enterostaminine that actually affect the stem cell niche, you can bypass cell therapy and allow the niche to do its job in a better way,” said Fiorina. “This approach could reshape the way we imagine cell therapy. I think that many other hormones with similar functions will be discovered.”
Fiorina is also exploring new treatments for diabetes itself. Under an agreement with Fate Therapeutics, his lab will investigate the ability of both genetically engineered and pharmacologically modulated blood stem cells to curb the autoimmune activity that destroys pancreatic beta cells.
Thus far, their mouse data indicate that the genetically engineered cells home to the pancreas, reduce abnormal immune-cell activity and reverse hyperglycemia, and that cells modulated with drugs have the same immune-regulating properties as the genetically engineered cells.
The study’s co-first authors are Francesca D’Addio of Boston Children’s Hospital and Ospedale San Raffaele in Milan, Italy, and Stefano La Rosa of Ospedale di Circolo in Varese, Italy.
The study was supported by the Italian Scientists and Scholars of North America Foundation (ISSNAF), the Minister of Health of Italy (grants RF-2010-2314794 and RF-2010-233119), the American Diabetes Association, an EFSD/Sanofi European Research Programme and the American Heart Association.
Adapted from a post on Vector, the clinical and research innovation blog at Boston Children’s.