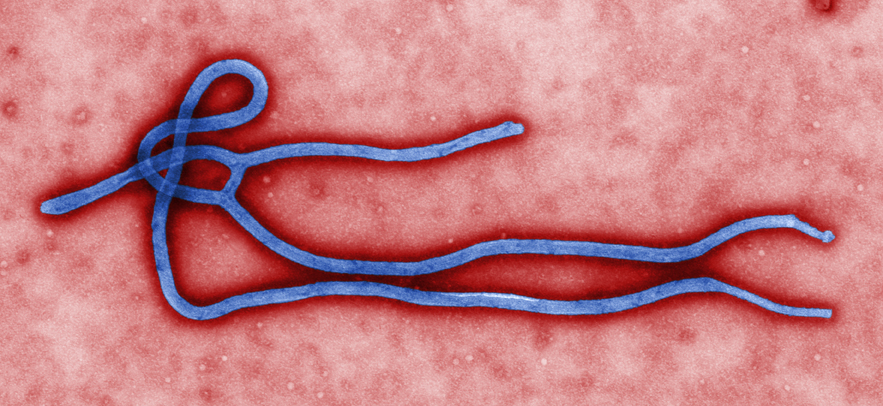
The Ebola virus. Image: CDC
While most primary care physicians responding to a survey taken in late 2014 and early 2015 expressed confidence in their ability to identify potential cases of Ebola and communicate Ebola risks to their patients, only 50 to 70 percent of them gave answers that fit federal guidelines when asked how they would care for hypothetical patients who might have been exposed to Ebola.
In addition, those who were least likely to encounter an Ebola patient—based on their location and characteristics of their patients—were most likely to choose aggressive management of patients who were actually at low risk.
The results of the survey, conducted by a team of Harvard Medical School investigators at Massachusetts General Hospital, have been published in the Journal of General Internal Medicine.
“Our findings demonstrate significant variation in how doctors make decisions in situations of uncertainty and show how decision making can be shaped by geography, sources of information and other factors,” said Ishani Ganguli, HMS instructor in medicine at Mass General and corresponding author of the report.
“They suggest that we need to do a better job helping doctors on the front lines of patient care deal with future global epidemics,” he said.
Ganguli and her colleagues noted that while only four cases of Ebola were diagnosed in the U.S. during the recent outbreak in West Africa, the extensive attention given to the dangerous disease by both the news media and governmental entities was followed by inappropriate measures.
For example, health workers were quarantined after returning from international relief efforts, even though their lack of symptoms indicated they were not infectious. People who had traveled to Ebola-free areas of Africa also saw their contact with other people restricted.
Physicians also overreacted, with 75 percent of the calls they made to the U.S. Centers for Disease Control and Prevention being about patients with no risk of having contracted Ebola.
Designed to assess how well primary care physicians across the country were prepared to handle potential Ebola risk, the survey was emailed to more than 460 internists and geriatricians early in December 2014 and remained available until mid-January 2015.
The 23 questions assessed the likelihood that providers might see patients at risk for Ebola and asked them to assess their own risk of exposure, how prepared they felt to identify possible cases or inform patients about Ebola risks, their sources of information about Ebola, whether their institutions had developed protocols for Ebola diagnosis and treatment, and other factors.
Respondents were also asked what measures they would take if consulted by patients who had returned from Ebola containment efforts in Sierra Leone either 10 or 28 days earlier or who worked in a hospital where an Ebola patient with whom they had no contact was receiving care.
Another question asked them to indicate whether patients with flu-like symptoms and meeting other criteria, including volunteering in an Ebola treatment center or visiting South Africa, were more likely to have influenza or Ebola.
In all of the described situations, the hypothetical patients had little and often no likelihood of having been exposed to Ebola.
Among the 202 primary care physicians who responded to the survey, 95 percent felt very prepared or somewhat prepared to identify a possible case of Ebola and 97 percent felt very or somewhat prepared to inform patients about Ebola risk. But their actual knowledge about how concerns about Ebola should affect their management of specific hypothetical patients showed considerable variation.
For example, when asked about a patient with flu-like symptoms who had recently returned from South Africa, 24 percent indicated that Ebola was the more likely cause, even though there have been no cases of Ebola in that country.
In their responses to questions about the transmission risks or the incubation period of Ebola, 20 percent said they would have chosen management approaches that were overly intense.
Those responses varied depending on the actual likelihood of a physician’s encountering an Ebola patient.
Three percent of those most likely to see such patients chose excessive management, while 23 percent of those with no possibility of seeing an Ebola patient took an overly intense approach.
“It could be that those not working in areas where they might encounter Ebola received less information from their institutions or local government sources, making them more fearful of the disease and more aggressive in evaluating potential cases,” Ganguli said.
“While 88 percent did report having consulted the CDC guidelines on Ebola at least once during the preceding year—and the CDC was the most commonly cited source of information—our results suggest the need to provide additional resources, like decision support hotlines,” she said.
The results also suggested that physicians might be swayed by media reports on outbreaks like Ebola, which Ganguli said places even greater importance on responsible reporting by news media.
“It would be interesting to investigate the reasons why some doctors would decide to test low-risk patients for Ebola or send them to the hospital, and to determine the real impact of misplaced concern about Ebola in terms of both resource allocation and delayed diagnosis of a patient’s real illness,” Ganguli said.
Adapted from a Mass General news release.